WHY LUMENIS
Over 50 years of industry leadership and innovation
Lumenis develops life-changing, minimally invasive solutions for the Aesthetic and Vision markets. We create and commercialize innovative energy-based technologies that enable a variety of skin, body, and eye care treatments. Lumenis has successfully introduced solutions for previously untreatable conditions and designed advanced technologies that have revolutionized existing treatment methods. We are BeautyTech pioneers, empowering people by broadening the horizons of health and celebrating beauty that matters.
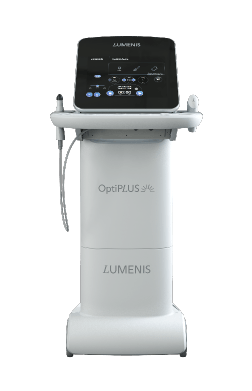
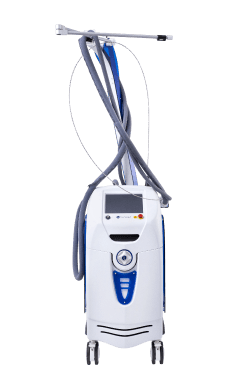
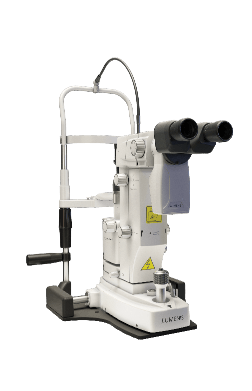
OUR PRODUCTS
YOUR SUCCESS
IS OUR MISSION
Every decision and device at Lumenis centres on you and your ability to change people’s lives.
Day in and day out, we’re committed to #CelebratingYou and the difference you make.
INDUSTRY
BEST
We are pioneers and leaders within the aesthetics and vision industries, bringing the most expansive expertise in energy-based treatments to the field.
As a Lumenis partner, you are equipped with the confidence that you are providing the very best that technology has to offer.
PIONEERING
INNOVATION
For over 50 years, Lumenis has revolutionized the Aesthetic and Vision domains by developing innovative energy-based solutions, including Laser, Intense Pulsed Light (IPL) and Radio Frequency (RF). We are passionate innovators, empowering our customers and patients worldwide.
WE’RE HERE TO HELP WITH ANY QUESTIONS
Please fill out our form,
and we’ll get in touch shortly.